Guide to the Skin Microbiome: Everything You Need to Know about Your Skin’s Invisible Guardians

What are microbiota and microbiome?
You’ve probably heard that bacteria live on our skin, but did you know they actually form an entire little world? Before we go further, let’s clarify two terms that are often mixed up.
Microbiota refers to all the living microorganisms on and in our body – bacteria, fungi, viruses, and other tiny “residents” we can’t see with the naked eye. Microbiome, on the other hand, is a broader concept. It’s basically the microbiota plus everything they produce: their genetic material and the way they interact with our body.
Our skin is home to millions of microorganisms that make up the skin microbiome, with a density that can reach up to a million bacteria per square centimeter. To put that in perspective – more microorganisms live on the surface of your skin than there are people on the planet! But before you get worried, it’s important to know that these microbes are actually our friends and allies.
What are microbiomes and how do they relate to facial skincare?
Now that we understand the basics, the question arises: why should we even care about something we can’t see? The answer is simple – the microbiome is actually your most important partner in maintaining healthy skin. The microorganisms that live on your skin are not just passive tenants. They actively participate in protecting your skin, helping it recover, regulating inflammation, and even influencing how your skin looks and feels.
When you use skincare products, you’re not just caring for the surface – you’re also affecting this delicate ecosystem of microbes. Every product you apply to your face can support or disrupt your microbiome’s balance. Research shows that a healthy, balanced skin microbiome contributes to a strong skin barrier, more robust skin immunity, and a youthful appearance.
That’s why caring for the microbiome has become a new paradigm in skincare. We no longer see skin only as a physical barrier, but as a dynamic ecosystem that requires careful nurturing and balance.
What exactly is the skin microbiome and what is its role?
Let’s dive a little deeper into this fascinating world. The skin microbiome is a living community that covers every inch of your skin. This community isn’t made up of just bacteria – there are also fungi, viruses, and other microorganisms all creating a complex ecosystem together.
What’s particularly interesting is that the microbiome isn’t the same on all parts of the body. In oily areas of the face, like the T-zone, one group of microbes predominates, while in dry areas, like the cheeks, a completely different set thrives. Even your armpits have a different microbiome than your hands. This diversity isn’t by chance – each area of skin has specific conditions (moisture, oiliness, temperature, pH) that determine which microbes will “prosper” there.
Key roles of the skin microbiome
- Protection. The microbiome acts as the first line of defense against harmful microbes. How? Beneficial bacteria “take up space” on the skin, preventing harmful bacteria from settling in.
- Production of natural protective substances. Many skin bacteria produce antimicrobial compounds that directly kill harmful microorganisms. Some strains make substances that inhibit pathogens, acting like natural antibiotics.
- Communication with the immune system. The microbiome is constantly “talking” to our immune cells, training them to recognize the difference between friends and foes. This communication is crucial to prevent excessive inflammatory responses that can lead to issues like eczema, acne, or psoriasis.
- Maintaining the skin barrier. Microbes help produce key components that strengthen the skin’s protective barrier, aid in retaining moisture, and block harmful substances from penetrating into deeper layers.
When and how does the skin microbiome develop?
Many people think babies are born with completely sterile skin, but the reality is much more fascinating. The process of skin colonization by microbes actually starts at birth, and this first contact with microbes is crucial for developing a healthy immune system.
- Birth – the first meeting with microbes. The way a baby is born has a big impact on which microorganisms they encounter first. Babies born vaginally come into contact with the mother’s vaginal and gut microbes. Babies born by C-section first meet the microbes in the hospital environment and on the skin of medical staff. You can notice differences in the first weeks of life, but they tend to diminish over time as the baby encounters microbes from their surroundings.
- The first year of life – setting the foundation. During the first year, the skin microbiome undergoes dramatic changes. At first, baby’s skin is colonized by bacteria from the Staphylococcus and Streptococcus genera. As the child grows, this community becomes more diverse and specialized for different parts of the body. By the end of the first year, the skin microbiome already shows characteristics specific to different body areas. What happens during this period is incredibly important. Early contact with a variety of microbes “trains” the baby’s immune system to distinguish good microbes from harmful ones. Research shows that disruptions in early microbiome development can be linked to an increased risk of allergies, atopic dermatitis, and other skin problems later in life.
- From childhood to adulthood. After the first year, the skin microbiome becomes more stable, but it continues to evolve throughout childhood and adolescence. Puberty brings major changes – increased sebum production (the oil that protects the skin) creates a new environment that favors different microbes. This is one reason why many teenagers experience acne during this period – shifts in the microbiome accompany hormonal changes. In adults, the skin microbiome is relatively stable but not static. It still adapts to conditions – changes in climate, diet, stress, products we use, and many other factors all influence it.
- Age and the microbiome. As we get older, the skin microbiome goes through changes again. In older people, microbiome diversity decreases, which can contribute to increased skin sensitivity and slower regeneration. This is one reason why caring for the microbiome is especially important as we age.
What does a balanced skin microbiome look like?
When the skin microbiome is functioning well, you might not notice it – and that’s actually a great sign! A balanced microbiome works quietly in the background, protecting your skin and keeping it healthy.
How does healthy skin with a balanced microbiome behave?
- Strong natural barrier. Your skin retains moisture well and isn’t too dry or too oily. It doesn’t feel tight after washing, and it recovers quickly from minor irritations.
- Resilience. Your skin doesn’t overreact to every new product or small change in diet or weather. It can adapt without drastic reactions.
- Stable through hormonal changes. Hormonal fluctuations don’t cause major issues. Breakouts and redness are rare and go away quickly.
- Healthy appearance. Your skin has a natural glow (not a greasy shine), an even tone and texture. It looks well-nourished and firm.
What does research say at the microscopic level?
- High diversity of species. A healthy microbiome has many different types of microorganisms. This diversity is like a rich forest – the more varied, the more stable and resilient the ecosystem.
- Dominance of beneficial bacteria. In a healthy microbiome, beneficial bacteria dominate. For example, certain strains of Staphylococcus epidermidis and Cutibacterium acnes (yes, some strains of C. acnes are actually good for the skin!) help keep things in balance.
- Balance, not absence of pathogens. Even a healthy microbiome contains some potentially problematic microbes. The key is that they’re present in small numbers and kept in check by the good bacteria.
- Stability over time. A healthy microbiome remains relatively stable. Small changes in diet or environment don’t cause drastic shifts in the microbial community.
What does an imbalanced skin microbiome look like?
Opposite to the balanced state, when the microbiome is disrupted – what we call a “dysbiosis” – your skin usually makes it very clear.
Visible signs of imbalance
- Frequent inflammation and irritation. The skin often reacts with redness, stinging, or itching. These reactions can be occasional or constant.
- Worsening of existing issues. If you have acne, eczema, or rosacea, these conditions become more pronounced and harder to control.
- Overly sensitive skin. Products that were fine before now cause reactions. The skin feels tight and irritates easily.
- Compromised barrier. Your skin feels dry and tight, or conversely – too oily and shiny. Moisture escapes more quickly; the skin may look thin and dull.
- Uneven tone and texture. You might see spots, bumps, increased flakiness, or even thickening of the skin.
What happens at the microbiome level?
Research shows that in a dysbiotic state, several characteristic changes occur:
- Reduced diversity. The number of different microbial species drops. The microbiome becomes “poorer” and more vulnerable to disruption.
- Overgrowth of certain species. Some bacteria or fungi start to dominate, replacing the beneficial ones. For example, with acne there’s often an overgrowth of certain inflammatory strains of C. acnes.
- Loss of helpful “guards”. The bacteria that produce protective substances and keep pathogens in check become fewer, leaving the skin unprotected.
- Changes in metabolite production. A disrupted microbiome produces different byproducts, including some that can further irritate the skin or damage the barrier.
So, when the microbiome is compromised, the consequences can be numerous.
- In acne, inflammatory strains of C. acnes take over, and protective bacteria are lost.
- In atopic dermatitis (eczema), we often see an overgrowth of Staphylococcus aureus, which worsens inflammation and damages the skin barrier.
- In rosacea, the “redness” intensifies due to shifts in microbial populations that lead to chronic inflammation and flushing.

What affects the skin microbiome?
Your skin microbiome isn’t static – it’s a living ecosystem that responds to many factors in our daily life. Understanding these factors helps us make better skincare choices.
Skincare products
Every time you apply something to your face, you’re affecting your microbiome. Some products support a healthy microbiome, while others can disrupt its balance:
- pH of the product. Skin is naturally slightly acidic (around pH 5.5), which beneficial bacteria favor. Products that are too alkaline can disturb this balance.
- Harsh cleansers. Strong cleansing agents with many active ingredients can wash away not just dirt but also helpful microorganisms, leaving the skin unprotected.
- Antibacterial ingredients. These can be a double-edged sword – while they kill harmful bacteria, they often also kill beneficial ones. This can create a gap that pathogens can fill.
Lifestyle and habits
Your daily habits have a direct impact on microbiome health:
- Diet. What you eat has a major effect. While it’s well-known that diet influences the gut microbiome, it also indirectly affects your skin through various mechanisms.
- Stress. Stress isn’t just in your head – it directly affects your skin and its microbiome. Chronic stress can change microbiome composition and weaken the skin barrier.
- Sleep. Sleep is when skin regenerates. Not getting enough or having poor quality sleep can weaken the microbiome and reduce its ability to recover.
- Exercise. Physical activity generally has a positive effect on the body, including the skin microbiome. However, excessive sweating without proper cleansing afterward can cause issues.
Environment
Your environment constantly influences your skin microbiome:
- Climate conditions. Humidity, temperature, and sun exposure affect which microbes thrive on your skin. You might notice that your skin behaves differently in winter versus summer.
- Air quality. Pollution, smoke, and other airborne irritants can damage the skin barrier and microbiome.
- Contact with nature. People who spend more time outdoors tend to have a more diverse microbiome.
- Frequency of washing. Overdoing showers or face washes, especially with hot water, can upset the skin’s natural balance.
Factors that can damage the skin microbiome
While some factors simply influence the microbiome, certain situations can cause serious damage. Let’s list the most common “culprits.”
- Antibiotics – the necessary evil?
Antibiotics are life-saving medicines, but their use comes at a cost to our microbiome. When you take an antibiotic (by mouth or apply it to the skin), it doesn’t distinguish between “good” and “bad” bacteria – it destroys them all.- Oral antibiotics. Systemic antibiotics affect the entire body, including the skin microbiome. After a course of antibiotics, the skin microbiome may take weeks or even months to recover.
- Topical antibiotics. Applied directly to the skin, these can target acne or infections, but long-term use can lead to resistance and imbalance.
- Harsh skincare products.
The modern cosmetic industry offers many products, but not all are friends to your microbiome:- Strong chemical peels or exfoliants. They can be helpful in moderation, but frequent or aggressive use can harm the living layer of microbes on your skin.
- Alcohol-based products. These completely dry out the skin and destroy the microbiome. They may temporarily reduce oiliness, but in the long run they cause more problems.
- Products with extreme pH. These disrupt the natural acidity of the skin, creating an unfavorable environment for beneficial bacteria.
- Lifestyle and habits.
Some of our daily behaviors can harm the microbiome, often without us realizing it:- Touching your face with dirty hands. This transfers various microbes (and dirt) to your facial skin, which can upset the balance.
- Excessive hygiene. Ironically, being too clean can be a problem. Constantly washing hands with antibacterial soap or over-washing your face can do more harm than good.
- Smoking. It damages the skin in many ways, including negatively affecting the microbiome.
- Poor diet. A diet high in processed sugars, unhealthy fats and low in nutrients can harm the microbiome.
- Chronic stress. It’s not just a feeling – it triggers hormonal changes that directly affect the skin barrier and microbiome.

How long does skin microbiome regeneration take?
One of the most common questions people ask is: “If my microbiome is disturbed, how long will it take to recover?”
Short answer: It depends on many factors, but in most cases you can expect initial improvements after a few weeks of proper care. However, complete regeneration and stabilization of the microbiome can take several months.
More detail:
- First weeks (1–2 weeks). This is the “calming down” phase. When you start using gentler products and stop aggressive treatments, your skin will first halt acute reactions. Redness and irritation should decrease. During this time the microbiome begins to stabilize, but it’s not yet fully restored to its optimal state.
- Middle period (3–8 weeks). During this time the microbiome actively regenerates. Beneficial bacteria start to return and reclaim their positions. You may notice your skin’s texture improving, fewer pimples, or less sensitivity.
- Longer term (2–6 months). Complete stabilization and achieving a new, healthy balance can take several months. Your microbiome not only recovers but also “learns” – forming a new stable state that is more resilient to future disruptions.
Factors affecting recovery speed:
- Extent of damage. If you only used mild products that slightly disturbed the balance, recovery will be faster than after intense treatments or long-term antibiotic use.
- Your age. Younger skin typically regenerates its microbiome faster than older skin.
- Overall health. If your body is healthy, with a strong immune system and balanced hormones, your microbiome will recover more quickly.
- Consistency of care. If you frequently change products or alternate between aggressive and gentle products, recovery will be slower.
- Lifestyle. Chronic stress can significantly slow down regeneration.
- Diet and hydration. Proper nutrition and sufficient water intake help the recovery process.
What you can do to speed up the process:
You can’t force the microbiome to regenerate overnight, but you can create optimal conditions:
- Be patient and consistent. The worst thing you can do is constantly change products or try new treatments while the microbiome is recovering.
- Simplify your routine. Use the minimum number of products needed – a gentle cleanser, a quality moisturizer, and a sunscreen.
- Avoid extremes. Don’t use products that are too aggressive or too occlusive.
- Watch your diet. Eat a varied diet rich in fiber, fermented foods, and antioxidants.
- Manage stress. Find ways to reduce stress – meditation, yoga, walks in nature, or any methods that work for you.
When do you need a dermatologist if your microbiome balance is off?
This is an important question because sometimes it’s hard to tell the difference between a “normal” imbalance you can fix yourself and a more serious problem that needs professional help.
When you can handle it yourself
There are situations where you can try to restore balance on your own:
- Mild irritation or dryness after a new product. If you stop using that product and your skin calms down in a few days, you probably don’t need to visit a dermatologist.
- Seasonal changes. If your skin reacts to changes in seasons (e.g., becoming drier in winter), this is normal, and you can adjust your skincare routine accordingly.
- Occasional breakouts. Those are normal and don’t necessarily mean your microbiome is out of balance.
- Temporary flare-up after stress or lack of sleep. If the problem is short-lived and quickly passes, it usually doesn’t require a doctor’s intervention.
When it’s time for a dermatologist
Certain signs indicate that the issue might be more serious and you should seek professional help:
- Persistent symptoms that worsen. If you’ve adjusted your skincare for several weeks but your condition doesn’t improve or even gets worse, it’s time to see a dermatologist.
- Sudden lots of pimples or acne. This isn’t just a cosmetic issue – it could indicate a hormonal imbalance that requires medical intervention.
- Signs of infection. Spreading redness, pus-filled bumps, painful patches, swelling – these are signs that harmful bacteria have taken over and it’s beyond simple skincare fixes.
- Chronic eczema or dermatitis. If your skin constantly itches, peels, cracks, or bleeds, you should definitely see a doctor.
- Drastic skin changes. If your skin changes dramatically without an obvious reason (no new products, no unusual stress), it could indicate an underlying health issue.
- Impact on quality of life. If the skin problem affects your mental health, confidence, or daily activities, don’t wait – seek help.
What to expect from a dermatologist
A dermatologist will:
- Examine your skin thoroughly and may take samples for analysis if they suspect an infection or specific issue.
- Ask about your skincare routine, products used, lifestyle, diet, and medical history.
- Possibly prescribe specific treatments – these could be topical or oral medications, special cosmetic products, or changes to your routine.
- Give advice on how to support your microbiome’s recovery along with any medical treatment.
- It’s important to understand that a dermatologist isn’t just treating symptoms but also helping identify the root cause of the problem to prevent its recurrence.
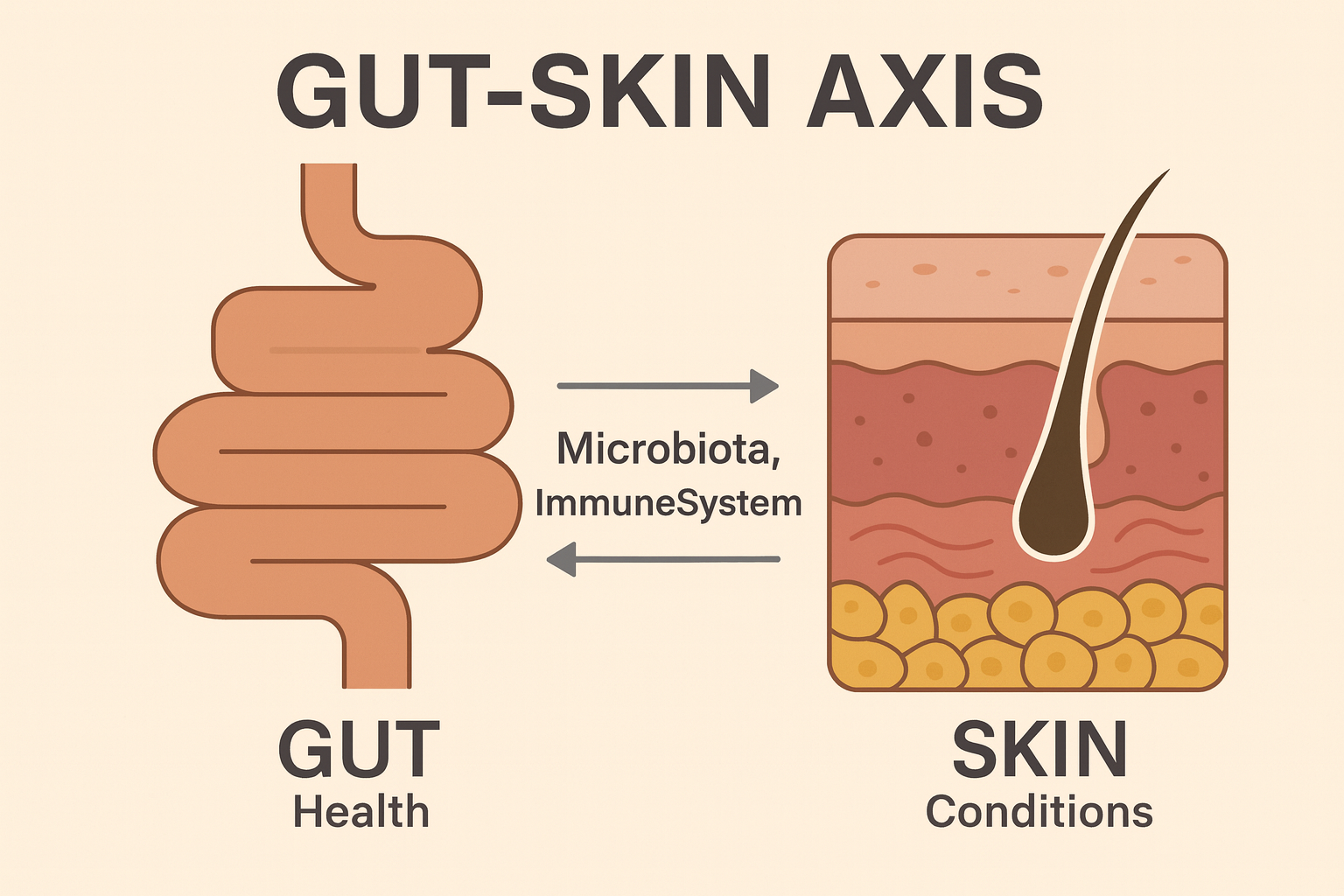
Does the gut microbiome affect the skin microbiome?
This is a fascinating question that reveals one of the most exciting areas of modern dermatology – the gut-skin axis. It might seem strange that what happens in your stomach can affect your skin, but the connection is not only real, it’s incredibly strong and complex.
How the gut communicates with the skin
- Through the immune system. About 70% of our immune system is located in the gut. When the gut microbiome is healthy, it “trains” immune cells to respond appropriately. These cells then travel through the body, including to the skin, where they help maintain a healthy microbiome and prevent inflammation. When the gut microbiome is disrupted (for example, by antibiotics or poor diet), the immune system can become “confused” and overactive. This can lead to inflammation not only in the gut but also in the skin.
- Through gut inflammation. A disrupted gut microbiome can allow bacteria and their products to leak through the gut lining into the bloodstream. This triggers inflammation throughout the body, including in the skin.
- Through metabolites. Gut bacteria produce thousands of different compounds. Some of these, like short-chain fatty acids (SCFAs), travel through the bloodstream and influence skin health. These compounds help regulate skin inflammation, strengthen the skin barrier, and even affect sebum (oil) production.
- Through hormones and neurotransmitters. The gut produces neurotransmitters (like serotonin) and hormones that can affect the skin. Stress affects the gut, the gut affects hormone production, and hormones affect the skin – it’s all connected!
Specific examples of the gut-skin link
- Acne. Studies show that people with acne often have an imbalanced gut microbiome. Improving gut health through probiotics or dietary changes can help restore the gut microbiota, which in turn can benefit the skin.
- Atopic dermatitis (eczema). There’s a clear link between a disrupted gut microbiota and eczema. Sometimes acne or eczema can be a sign of an overall system imbalance starting in the gut.
- Rosacea. Patients with rosacea often have gut issues like SIBO (small intestinal bacterial overgrowth). By restoring balance in the gut, we can improve symptoms that show up on the skin.
- Psoriasis. This autoimmune condition also shows a strong connection with the gut microbiome. Balancing the gut microbiota can help control its symptoms.
How to support the gut-skin axis
- Eat fermented foods. Yogurt, kefir, buttermilk, sauerkraut, kimchi – these foods introduce beneficial bacteria to your gut.
- Include prebiotics. These are fibers that serve as food for good bacteria. They’re found in onions, garlic, bananas, and whole grains.
- Avoid over-processed foods. Excess sugar and heavily processed foods can harm the gut microbiome.
- Consider probiotics. While not a cure-all, certain probiotic supplements can help, especially after antibiotics.
- Manage stress. Stress directly affects the gut (remember “butterflies in the stomach”), which then shows up on the skin.
Strengthening the skin microbiome: how important is the skin barrier
The skin microbiome and the skin barrier are inseparable partners – one depends on the other, and when one suffers, the other does too. Understanding this relationship is key to healthy skin.
What is the skin barrier?
Think of your skin as a brick wall. The skin barrier is the outermost layer of that wall – it protects the inside from external factors and prevents moisture from escaping. This protective layer consists of several components:
- Skin cells (keratinocytes) that are tightly packed together to form a physical barrier.
- Lipids (fats) that fill the spaces between these cells and prevent water loss.
- Natural moisturizing factors (NMF) that attract and hold moisture in the skin.
- Acidic pH (around 5.5) that creates an unfavorable environment for harmful microbes.
- Microbiome on the surface, which actively contributes to defense.
How does the microbiome strengthen the skin barrier?
The relationship between the microbiome and the barrier is two-way and fascinating:
- Microbiome produces protective substances. Beneficial bacteria on our skin create compounds that help build and maintain the lipid layer. For example, certain bacteria produce ceramides – key fats for a healthy barrier.
- Microbiome regulates pH. Bacteria produce acids that maintain the skin’s optimal, slightly acidic pH. This acidic pH not only protects the skin but also favors beneficial bacteria.
- Microbiome stimulates regeneration. Microbes communicate with skin cells and encourage them to produce protective proteins and antimicrobial compounds.
- Microbiome “trains” the immune system. Helpful bacteria assist the immune system in distinguishing “bad” from “good” residents, preventing inflammatory reactions that could damage the barrier.
How does the skin barrier support the microbiome?
- Provides habitat. Different parts of the skin (dry, oily, moist) offer various niches for diverse bacteria.
- Supplies nutrients. Beneficial bacteria “feed” on sebum and other compounds secreted by the skin.
- Controls moisture. A healthy barrier maintains optimal humidity, which allows beneficial bacteria to thrive.
When the barrier is damaged, the microbiome suffers
- A damaged barrier loses moisture more quickly, creating unfavorable conditions for good microbes.
- It becomes more permeable to harmful microbes and allergens.
- Its pH may change, potentially favoring harmful bacteria.
- It produces fewer protective compounds.
This creates a vicious cycle: a damaged barrier leads to a disrupted microbiome, and a disrupted microbiome further damages the barrier.
How to support both the barrier and the microbiome
- Be gentle with your skin. Avoid aggressive skincare products that strip natural oils from the skin.
- Hydrate. Use products that replenish and lock in moisture.
- Mind the pH. Choose products with slightly acidic or neutral pH.
- Protect from the sun. UV rays damage both the barrier and the microbiome.
- Don’t overdo it. Using too many products or layers can be counterproductive.
How to balance/regulate the skin microbiome
Now that we understand what the microbiome is and how it works, let’s move to the practical part: what exactly can you do to help your microbiome return to balance?
First step: Stop doing what’s damaging it
Before adding anything new, the most important thing is to stop what caused the problem:
- Identify aggressive products. Look at your skincare products. If you’re using strong cleansers (with sulfates), products where alcohol is a main ingredient, or products with extremely high or low pH, it’s time to replace them.
- Reduce frequency. If you’re washing your face multiple times a day or exfoliating every day, scale back. Wash just in the morning and at night, and use gentle exfoliation only once a week.
- Simplify your routine. We often add more products when our skin has problems, but sometimes the solution is the opposite – use fewer, not more.
Second step: Create a favorable environment
Now that you’ve removed harmful factors, it’s time to create optimal conditions for recovery:
- Gentle cleansing. Use a mild cleanser. Ideally, one that has a pH close to the skin’s (around 5–5.5) and doesn’t foam much. Foam can be a sign of harsh surfactants. Wash your face with lukewarm water, not hot.
- Hydration is key. Hydration isn’t just about drinking water – it’s about locking moisture into the skin. Use a moisturizer that contains humectants (to attract moisture) and occlusives (to seal it in). Apply the moisturizer to slightly damp skin to “lock” the water in.
- SPF. UV rays not only damage the skin but also the microbiome. Daily sun protection is indispensable.
Third step: Active measures to strengthen the microbiome
Once you’ve set the foundation, you can consider products that actively support the microbiome:
- Probiotics and prebiotics in skincare. Probiotics in cosmetics can be live microorganisms (though rare, since keeping them alive in a product is difficult), their metabolites, or lysates (breakdown products). Prebiotics are ingredients that serve as “food” for good bacteria. Products with these ingredients can help restore balance.
- Fermented ingredients. Ingredients fermented by bacteria or yeast can be beneficial because they contain various compounds that support the microbiome.
Fourth step: Systemic support
The skin microbiome doesn’t live in isolation – it’s part of a larger system:
- Support the gut microbiome. Eat a varied diet, include fermented foods, fiber, and limit processed foods and sugar.
- Manage stress. Find techniques that work for you – meditation, exercise, hobbies, time in nature.
- Get enough sleep. Skin (and its microbiome) regenerates during sleep.
- Stay hydrated. Drink enough water – dehydration shows on the skin.
Fifth step: Patience and consistency
This might be the hardest, but it’s the most important step:
- Be patient. The microbiome won’t fix itself overnight. Give it time.
- Be consistent. Don’t change products or routines frequently. The microbiome needs a stable environment to recover.
- Track your progress. Keep notes on how your skin looks and feels. Sometimes changes are gradual, and you might only notice progress when you look back over weeks or months.
How does microbiome-focused skincare work?
Microbiome skincare is a new approach to skin care that differs from traditional methods. Instead of focusing only on “fighting” problems (like acne, blackheads, etc.), it focuses on “supporting” healthy skin.
What’s different in a microbiome-focused approach?
The traditional approach often says it’s okay to use aggressive ingredients (strong acids, high-concentration retinoids, antibiotics) to “attack” the problem. While these products can be effective in the short term, they often disrupt the microbiome and create new problems in the long term.
A microbiome-focused approach has a different philosophy: instead of destroying, it supports. The goal is to create an environment where good bacteria can thrive and harmful ones are naturally kept in check.
Key principles of microbiome skincare
- Respect the natural balance. Skin has its own ecosystem that has evolved over millions of years. Our job isn’t to “fix” it, but to support it. This means:
- Don’t wipe out all the bacteria. Even when you need to use antiseptics or antibiotics, use them targeted and short-term.
- Maintain the skin’s natural pH.
- Preserve the lipid layer that protects and nourishes the microbiome.
- Gentle cleansing. Cleansing is the most important step, but also the one most often neglected:
- Use gentle cleansers that don’t create a lot of foam.
- Wash your face only when needed (usually morning and night is enough).
- Use lukewarm water for washing.
- Don’t rub your skin with towels; pat it dry instead.
- Preserve and strengthen the barrier. A healthy barrier = a healthy microbiome:
- Use products that restore and hold in the skin’s moisture.
- Always use sunscreen.
- Avoid extreme cold or heat.
- Don’t exfoliate too often.
- Add probiotics and prebiotics. Products with probiotics or prebiotics can directly support the microbiome:
- Probiotics in cosmetics: These can be live microorganisms (rare, because it’s hard to keep them alive), lysates (broken-down bacteria), postbiotics (metabolites bacteria produce), or inactivated (heat-killed) bacteria that still have a beneficial effect.
- Prebiotics: Ingredients that serve as food for good bacteria, like certain sugars, fibers, or other nutrients.
- Avoid aggressive ingredients. Some ingredients are known to disrupt the microbiome:
- Strong antiseptics.
- High concentrations of alcohol.
- Very harsh surfactants.
- High concentrations of active ingredients without gradual introduction.
What does a microbiome-friendly daily routine look like?
Morning:
- Rinse your face with lukewarm water and a gentle cleanser (if needed).
- Apply a hydrating serum and moisturizer.
- Use SPF.
Evening:
- Gentle cleanse (if you wore makeup, remove it first with a gentle makeup remover).
- Use a serum or treatment if you have one (for example, products with pre/probiotics or antioxidants).
- Apply a moisturizing cream.
- Use an eye or anti-wrinkle cream if that’s part of your routine.
Once or twice a week:
- Gentle exfoliation (for example, a fine enzyme mask or a very mild chemical exfoliant).
- A soothing or hydrating mask (not a “deep cleanse” clay mask).
How do you know if a product supports the microbiome?
Look at the label or product description:
- Does it mention containing probiotics or prebiotics?
- Is it labeled pH-balanced or “skin’s pH”?
- Does it say “microbiome-friendly”?
- Does it avoid harsh surfactants and antiseptics?
Be careful: don’t just trust the marketing buzzwords. It’s best to research the brand and read reviews and user experiences.

Tips for preserving the skin microbiome
Now that you understand how microbiome skincare works, let’s talk about concrete daily tips to help maintain a healthy microbiome and prevent problems.
General daily tips
- Quality over quantity of products. It’s better to use 3–4 well-chosen products than 10 different steps. Each new product is a potential challenge for your microbiome, so keep your routine simple.
- Introduce new products gradually. When you want to try something new, don’t overhaul your entire routine at once:
- Introduce only one new product at a time.
- Use it for several weeks before adding another.
- Watch how your skin reacts.
- If you notice irritation, stop using that product and wait for your skin to calm down before trying again or switching to a similar product.
- Listen to your skin. Your skin tells you what it needs:
- If it feels tight and dry, it needs more moisture.
- If it’s oily and shiny, you might be over-hydrating or using products that are too gentle.
- If it’s irritated and red, you’re probably using something too harsh.
Tips for different skin types
- For dry skin:
- Avoid hot showers or washes – use lukewarm water instead.
- Use creamy, rich cleansers.
- Apply moisturizing products on damp skin.
- Consider adding a nourishing facial oil like immortelle oil to your routine.
- Use a humidifier indoors, especially in winter.
- For oily skin:
- Don’t over-clean; that can trigger even more oil production.
- Use lightweight moisturizers.
- Avoid heavy creams with harsh ingredients.
- If your skin remains excessively oily, consider consulting a dermatologist to check for hormonal or other issues.
- For sensitive skin:
- Choose products with few, gentle ingredients that nourish skin without being too aggressive.
- Avoid creams with perfumes or essential oils.
- Always patch-test new products on a small area of skin first.
- Be especially cautious with active ingredients (acids, retinol, etc.).
- For mature (aging) skin:
- Focus on hydration and locking in moisture.
- Use products with antioxidants (like vitamin C, E).
- Avoid overly aggressive anti-aging treatments that could damage the microbiome.
Important notes
- Listen to your skin: The timelines given here are approximate. Some people may take longer or shorter to restore their microbiome. It’s important to monitor your skin’s condition and see a dermatologist if needed.
- Be patient: Microbiome recovery isn’t done in 3 days. There might be periods where you see no progress, but stick with it.
- Seek help if necessary: If after weeks or months you don’t see improvement or if things get worse, it’s time to see a dermatologist.
- Individualize the approach: What’s written here is a general framework. Your skin may have specific needs that require a different care plan.
Conclusion
The skin microbiome is a fascinating world that has long been invisible to us, but it has a huge impact on the health and appearance of our skin. Understanding that we are not alone – that we carry with us millions of tiny helpers who protect our skin, regulate inflammation, and contribute to our well-being – changes how we approach skincare.
Instead of waging war on bacteria, we choose cooperation with them. Instead of aggressive treatments that “cleanse” and “sterilize,” we choose gentle care that supports the natural balance. Instead of ignoring the connection between our diet, lifestyle, and skin, we recognize that everything is interconnected.
Caring for the microbiome isn’t complicated – it’s often simpler than traditional approaches. It requires patience, consistency, and respect for the body’s natural processes. But the results – healthier, more resilient, and more beautiful skin – are worth the wait.
Remember: your skin isn’t just a surface – it’s a living ecosystem that deserves attention, respect, and care that acknowledges its complexity and beauty.
